Since 1960, the global population has been increasing by a billion every 10–15 years. If the trend persists, by 2024 the number of people living on our planet will hit 8 billion. At the same time, the global average life expectancy keeps increasing: since 1900 it has doubled and is now close to 70 years. In 1995–2016, the average life expectancy in Russia increased by almost 5 years.
According to scientists, in two decades or so, people could live to be two hundred and more years of age.
According to the WHO data for 2015, Russia ranked 109th in the world with an average life expectancy of 70.5 years, while the longest and the shortest average lifespan were seen in Switzerland and Sierra Leone (83.1 years and 50.1 years, respectively).
These trends are largely due to improvements in healthcare. On top of that, a British gerontologist Aubrey de Grey, one of the world's most renowned pioneers of anti-aging research, claims that in two decades or so, people could live to be two hundred and more years of age. To achieve this impressive result, he is going to use radical rejuvenation, a technology he has been working on for the last 20 years. A range of ways to “radically repair the human body” will undergo clinical human trials in the next two years. These technologies are part of the so-called engineering approach to curing aging, which provides for repairing the damage in due time using replacement parts rather than editing human genomes. And it can also be done through medical therapy programmes.
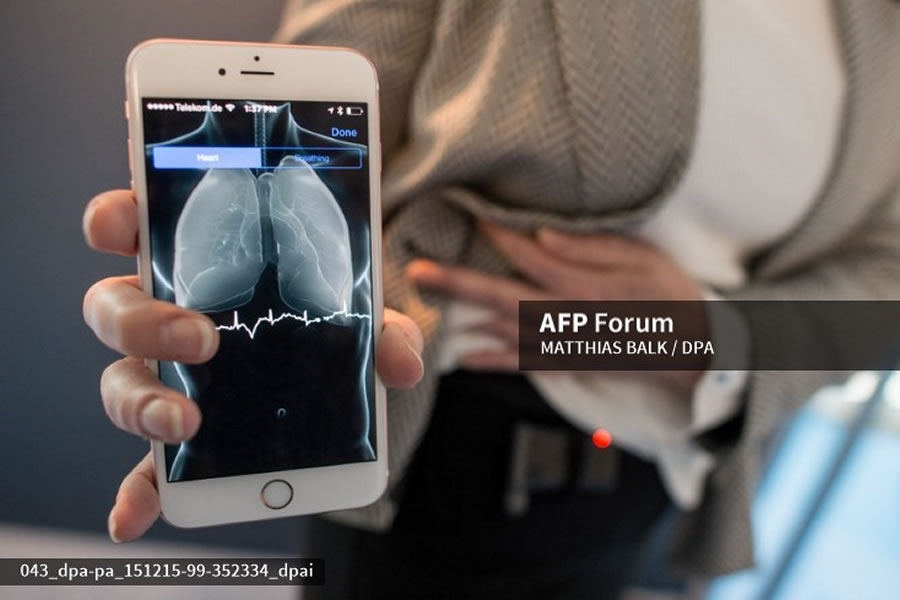
The telemedicine law enables Russian doctors to provide services remotely – over the phone or online.
No doubt, healthcare will keep developing fast. Experts distinguish several key trends that are important for many producers of petrochemicals, one of the main industries that supplies products suitable for a variety of medical applications.
Remote aid
The telemedicine law that came into effect in 2018 enables Russian doctors to provide services remotely – over the phone or online. Telemediсine technologies can now be applied in giving first, emergency, specialised, hi-tech aid and palliative care. Doctors can hold remote meetings to seek advice from more experienced colleagues or experts from dedicated medical research institutes. An integrated electronic system available to all registered healthcare providers will store data on every patient, enabling remote health monitoring and e-prescribing.
Medical wearables uses to constantly monitor the person’s condition.
Another increasingly important trend in the next-generation healthcare is personalised medicine. Collecting, storing and analysing health data on every patient pave the way for better diagnosis and tailored treatment.
The market is seeing an increasing number of medical wearables, such as bracelets, body sensors, contact lenses, and implants used to constantly monitor the person’s condition (pulse, blood pressure, metabolic markers, etc.). By 2035, the 24/7 monitoring system will cover the majority of Russians, which will help provide emergency care, promptly identify risks and predictors of sequelae and exacerbations and carry out routine activities as scheduled.
According to Research and Markets, medical wearables revenue will grow by 21.3% to USD 41.3 bn between 2016 and 2020. In 2021, the number of shipments will reach 33 million vs 8 million in 2016, says ABI Research. Those devices include:
• monitoring systems (cardiac and brain activity, blood pressure, glucose levels, sleep metrics, etc.);
• multi-parameter monitoring systems;
• systems for remote interaction with doctors;
• wearable, implantable and swallowable sensors for a range of health metrics;
• diagnostic and rapid analysis systems (blood, saliva, breathing, etc.);
• elderly, chronic and child care systems;
• health and medication control and treatment planning apps, smart coaching systems, etc.
Russia's medical products market worth some RUB 445 bn offers a huge potential, with a mere 10–20% of its capacity exploited, according to various estimates. By 2020, the share of Russian products should increase from 21% to 40%, as stated in the government programme for the development of the pharmaceutical and medical Industry (Pharma 2020). The medical industry development strategy until 2020 approved by the Ministry of Industry and Trade in 2013 stipulates that basic medical services should be provided using domestically manufactured equipment.
70%
A decrease in the number of US outpatients eight years after telemedicine became available. The same period saw the number of hospitals shrink by one fourth.
According to PwC, healthcare is among the five most promising industries in terms of petrochemical consumption, with 81% of domestic top managers surveyed in late 2017 pointing at a growing demand from medical companies and healthcare providers.
In April 2018, there were some 400 medical product manufacturers in Russia. Each year, they need more petrochemical supplies to address a wide range of medical challenges. Those include polymers, ceramics, composite materials and rubbers. Some of the most sought-after products are basic polymers, such as silicones, polyurethanes and polyolefins, along with polyethylene, polymethyl methacrylate, polystyrene, polypropylene, hydrogels, polyacrylate, various plastics, polycarbonate, kapron and others. All of them must meet increasingly tough requirements to their properties, from weight, strength and elasticity to biocompatibility and bioinertness. The market is also looking for better plastics and ceramics that will serve as more efficient substitutes for traditional metals. Biopolymers with wide industrial applications will be enjoying strong demand as well.
Manufacturers are in need of raw materials and equipment
Yuri Vlasov,
Head of Production, MedProm Bobeny Production:
Russia's medical products market worth some RUB 445 bn offers a huge potential, with a mere 10–20% of its capacity exploited.
«The most basic disposable syringe consists of two polymeric parts – a barrel and a plunger. The barrel can be manufactured using only special medical-grade raw materials (polypropylene in this case), whose main difference from their conventional counterparts is that they have a slip additive. It ensures smooth movement of the plunger during an injection, which is a critical quality of any syringe. Another additive required to make a barrel is the so-called nucleating agent. It makes the barrel's walls translucent and allows for the application of legible markings.
High-temperature injection moulding disinfects the material, eliminating the need for extra sanitising components.
At present, there are no Russian producers of slip additive containing polymers required for our products. However, it is not just the additive – it can only be applied using high-tech feeding equipment, the installation of which would require upgrades and significant investment, which is not yet a feasible option for Russian polymer producers. The switch to domestically produced raw materials could save a lot of money for the medical disposables industry, hence pushing down end product prices and helping squeeze Chinese products out of the market.
Another problem is the lack of Russian equipment to manufacture medical disposables and packaging, which is quite surprising given that it does not require the same kind of modification for medical purposes compared to the raw materials equipment. That makes it a problem of the entire polymer industry, not just medical product manufacturers.
Talent is also an issue, as there are no institutions providing relevant vocational training. As a result, we often have to train employees ourselves right at the workplace».
Now, correction the bite can be done with individual “aligners” – transparent fixing devices causing minimum inconvenience.
81% of domestic top managers surveyed in late 2017 pointing at a growing demand from medical companies and healthcare providers.
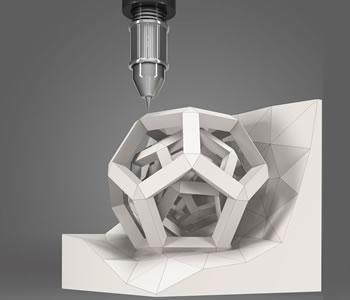
One of the facets of personalised medicine is creating artificial organs based on the patient’s gene map, and similar cross-technology projects. For example, 3D scanning and printing, advanced software and new polymers together have disrupted the dental industry. Once, painful procedures and surgery, including prosthodontic treatment, braces, etc. were needed in order to straighten one’s teeth or correct the bite. Now, it can be done with individual “aligners” – transparent fixing devices causing minimum inconvenience.
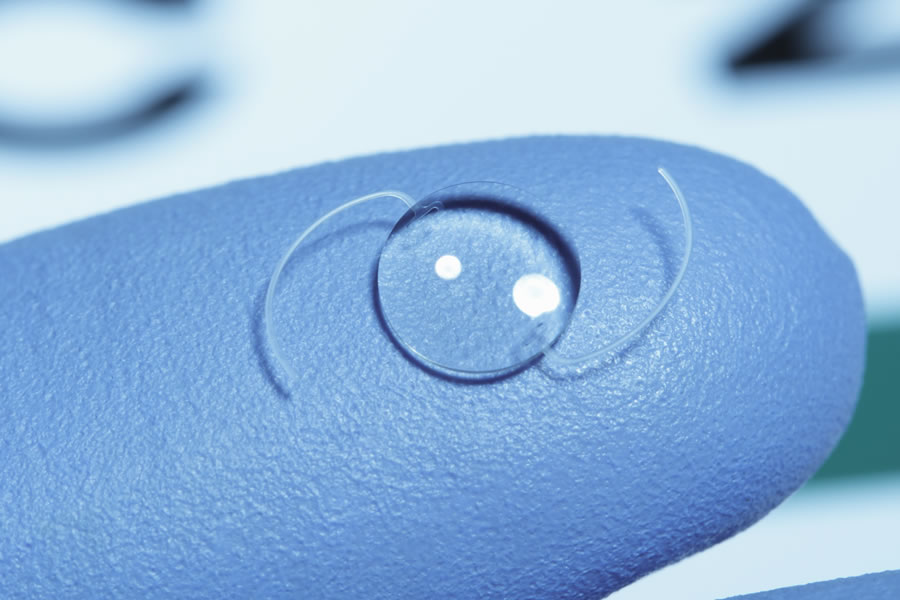
Companies focused exclusively on development of innovative materials for the medical industry are emerging. Entire organs or their fragments can be replaced using such materials. For quite a while already, ophthalmologists have been able to replace the lens using implantable lenses made of specially structured materials. In most cases, polymers substituting the lens do not cause any tissue reactions or rejection, with the patient's vision quickly returning back to normal.
Ophthalmologists have been able to replace the lens using implantable lenses made of polymers materials.
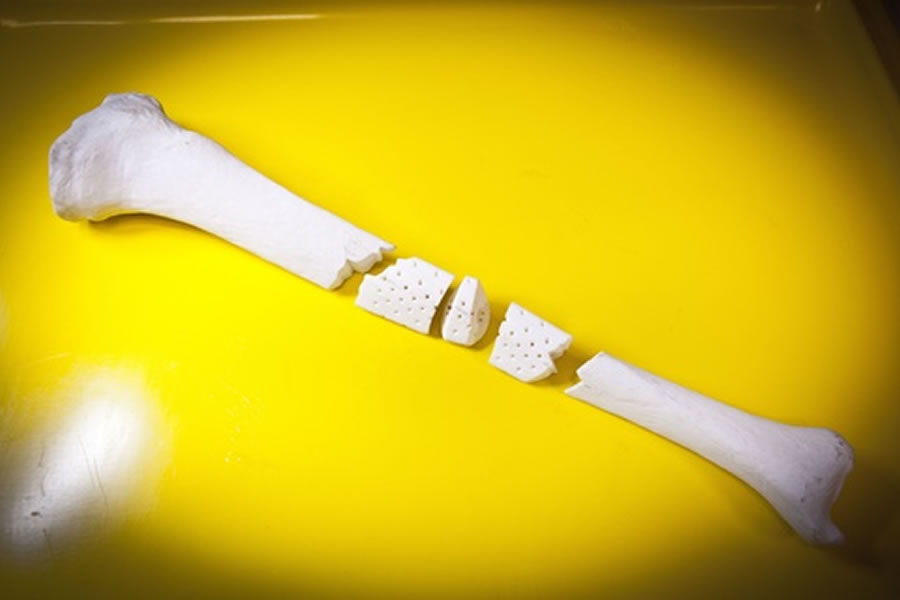
In 2016, 3D printing helped create artificial liver, arteries and bones. Not only did the organs not cause any problems after the transplantation, but they also developed their own vascular network. Soon, doctors will be able to replace any ailing or injured organ with a printed one based on the patient’s gene map. Moreover, 3D printers will make doses of medication according to individual schemes suggested by doctors.
Bones, which are considered a perfect composite thanks to their minerals and organic matter, can also be replaced with artificial counterparts. Polymers have extended the range of properties for materials used to make endoprostheses. One of them is HDPE, which can function in the same way as collagen. It makes prostheses as elastic as a living tissue – and it attaches to the bone tissue smoothly (the so-called osseointegration). Importantly, modern polymers have useful “prosthetic” lives of up to 30 years, saving patients the hassle of further surgery.
In 2016, 3D printing helped create artificial bones.
Yet another item on the agenda is cranioplasty, a skull repair technique. Russian specialists have contributed to this field by creating reperene prostheses. Strong and highly biocompatible and bioinert, reperene is ideal for closing smaller lesions. The perforated plate in the prosthesis soon gets filled with fibres of the restored tissue. Today, individual reperene implants are routinely used in surgery at the Burdenko Neurosurgery Institute, etc. Based on a spiral CT scan of the patient’s skull, a 3D model of the defect is created so that the implant could match the lesion as much as possible.
In April 2018, there were some 400 medical product manufacturers in Russia.
Demand for biomaterials
Currently, there is a strong demand for biopolymers that have a long lifetime or rapidly degrade into simple metabolites and are excreted in predefined times with no harm to a human body. They are often replaced with new tissues. For instance, researches from the Centre of Composite Materials at the National University of Science and Technology (MISIS) are developing shape memory implants that do not require fixation devices. Once a 3D-printed implant is installed and heated, it adheres to the bone and restores the damaged bone areas. Such implants use a biodegradable polylactide-based scaffold with live cells retrieved from the patient’s own bone marrow. Blood vessels and other tissues grow through this matrix, which dissolves at some stage.
Experts believe that ageing of the planet’s population and an increase in surgical interventions to replace tissues and organs will in the long run lead to a sustainably growing demand for biocompatible and biodegradable medical materials. GIA expects this global market to grow to USD 106.7 bn by 2020.
What healthcare needs from biocompatible materials
1) Biological compatibility with cells and the immune system. Healthcare needs materials with good cell adhesion properties that do not get rejected.
2) Mechanical properties comparable to natural materials. Healthcare needs materials that best mimic live organs (e.g. simulate appropriate tactile sensations for a limb) and provide comfort (e.g. lower mechanical stress on a body part that a prosthesis attaches to).
3) Biodegradability. Healthcare needs materials lasting from a week to a year (e.g. for post-surgery treatment). At present, the market is offering materials that degrade in a short (under a week) or long (9–18 months) time, but none with a lifespan between those.
3D printers will make doses of medication according to individual schemes suggested by doctors.
Targeted drug delivery
Another trend in today's healthcare is a strong focus of pharmaceutical producers on medicines for treating cancer and other rare or chronic diseases. This segment is growing fast, with new medicines and techniques to cure HIV and AIDS, cancer and other rare diseases emerging every year. It also receives support from the government. On top of that, the growing share of seniors in the world population and an increasing frequency of chronic diseases boost margins from these products.
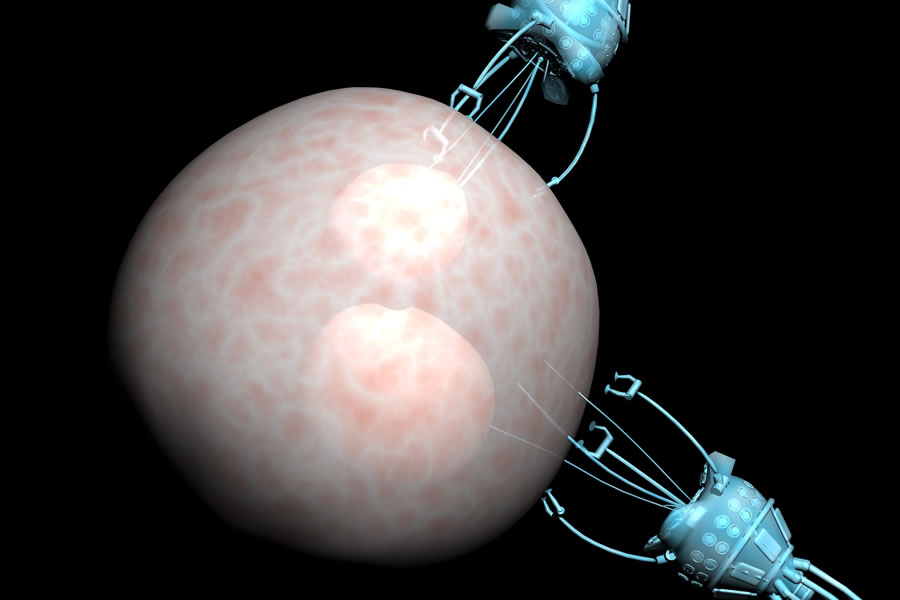
Like with many other diseases, extensive research here goes into targeted delivery systems that transport the drug straight to the affected part of the body, avoiding interaction with other areas or media (e.g. gastric acid). Smart delivery is extremely important in treating cancer when malignant cells proliferate fast and cannot be targeted by the needle.
In this context, a special focus is placed on nanomedicine that revolves around the idea of trapping active agents in a nano-sized container. Previously, the smart delivery technology used liposomes, spherical lipid bilayers encapsulating the drug. Liposome containers were good at delivering nano-medications to targeted areas, such as tumours, but failed to deal with poor solubility, which required more harmful solvents to be used. The solution to the problem was micellae, nano-sized particles based on polyoxyethylene and polyoxypropylene copolymers. They decrease the toxicity of drugs and allow for an increase in concentration.
Smart delivery is extremely important in treating cancer when malignant cells proliferate fast and cannot be targeted by the needle.
According to Transparency Market Research estimates, 2019 will see the global nanomedicine market expand to USD 175 bn. Successful developments in this area rely heavily on the optimal choice of chemicals, with polymer coatings becoming increasingly important in drug delivery systems. In addition to micelle production, polymers may be used to manufacture long-lasting medicated band aids (patients no longer need to remember to take their medicines), hydrogel-based sensors for continuous glucose monitoring for diabetic patients, etc.
Investment opportunities
Adel Gatin,
Chief Expert of the Finance and Economics Department at SIBUR, says:
“Petrochemical products, including those of SIBUR, are well-positioned to meet the requirements of today's healthcare. Our offering includes several products applied in this area. For example, special grades of polypropylene to produce syringes and non-woven fabrics used in disposable clothing for patients, and polyethylene terephthalate (PET) for blood collection tubes. Also, we are considering the options to use our polypropylene for packaging infusion solutions, and rubbers in medical products.
Speaking about healthcare of the future, we could make materials for polymer tablet coating in Dzerzhinsk or materials for implants from basic polymers. In two years, ZapSibNeftekhim, SIBUR’s facility under construction, will start producing a new product – high-density polyethylene (HDPE). Some of its grades will be used in medication packaging.
SIBUR’s offering includes special grades of polypropylene to produce syringes and non-woven fabrics.
Here we plan to focus on delivering unique properties, for example, selective solubility in various biological media, programmed degradation and compatibility with human cells. To achieve these goals, we need to partner with biologists and pharmacologists.”
Download PDF









What healthcare needs from polymer coating in drug delivery systems
1) Targeted delivery of drugs to diseased organs or tissues
2) Stability to prevent loss of the medication along the way
3) Smooth surface
4) Lower production costs