A virus is a non-cellular infectious agent that replicates only inside living cells. Once inside a human body, a new strain will launch an attack on the entire global population. Today, there are not many effective ways to combat viruses, but scientists continue the search, and the steps that are being taken in that direction clearly demonstrate the key role chemistry plays in the process.
Virus insurance
Vaccines are not a cure, but they remain the primary means of preventing a pandemic. The weakened virus contained in the serum enters the body and mobilises natural defences, which helps prevent the progression of the disease. The higher the vaccination rate, the lower the spread of the disease. But the truth is that any vaccine is created for a specific, already known virus. A universal remedy for all infections is a utopia. Moreover, viruses tend to mutate, which means that the active component of the vaccine has to be regularly updated. The coronavirus was first discovered and described in 1965, and since then it has been constantly mutating, going on the offensive at times. The Coronaviridae family is also blamed for the SARS outbreak of 2002 and the MERS outbreak of 2013. Vaccine for the type we are currently dealing with does not exist.
Vaccines are not a cure, but they remain the primary means of preventing a pandemic
Typically, making a vaccine can take years but in case of emergency all possible resources are mobilised. The current war on the virus (a pandemic in medical terms) forced the Russian Government to allocate additional resources from the Reserve Fund for vaccine research and testing drugs that could help fight the infection. Russia’s leading scientific groups and pharmaceutical companies have stepped up.
A team of the Smorodintsev Research Institute of Influenza has deciphered the full genome of the new coronavirus, which is central to developing drugs that will work. The institute is working on three concepts of the new vaccine. Time will tell which of them will be selected for production. In just two months, Vector virology and biotechnology centre created several prototypes of the future vaccine. Following the animal trials to be completed by the end of April, the most effective vaccine will be tested in humans. Scientists expect to proceed to this stage in early summer.
The Russian Government to allocate additional resources from the Reserve Fund for vaccine research and testing drugs that could help fight the infection.
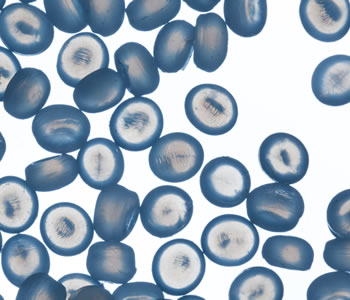
The Department of Virology of the Moscow State University suggests using drugs based on special spherical particles that can deliver active components
The Department of Virology of the Moscow State University suggests using drugs based on special spherical particles that can deliver active components. BIOCAD has started the development of its own coronavirus vaccine relying on previous research, as a tried and tested technology may help reduce the time needed for making a Russian formula. Scientists believe that a mass-produced vaccine will become available in late 2020 or early 2021.
Find and neutralise
Before the vaccine is created, scientists have yet to conduct a series of studies, obtain approval of the authorities and pass certification. But a way to identify the infection even in asymptomatic carriers and prevent its further spread already exists, and it is testing. Russia used to rely on a test system developed by Vector virology and biotechnology centre, but since early April these tests are performed with a new highly sensitive test system developed by Rospotrebnadzor’ Central Research Institute of Epidemiology.
A team of the Smorodintsev Research Institute of Influenza has deciphered the full genome of the new coronavirus, which is central to developing drugs that will work.
Sorting out terminology
Today, the official name for the new strain of coronavirus is SARS‑CoV‑2 (severe acute respiratory syndrome coronavirus).
According to WHO, the main coronavirus testing method is Polymerase Chain Reaction (PCR) testing (polymerase is an enzyme), which can detect the virus during the incubation period.
A swab fr om a person’s upper respiratory tract is taken and sent to the lab, wh ere it is exposed to special components. The envelope of the virus is destroyed, and a mix of DNA materials is left in the tube. Deoxyribonucleic acid (DNA) is a macromolecule that stores all biological information in the form of a genetic code. Coronavirus has specific blocks in its structure, and the lab technician synthesizes a small piece of his DNA as a model and looks for the same DNA in the mixture. If matches are found, then by multiplying the cell, you can see the presence of the virus, and this will mean that the person is infected.
Testing is recognised as one of the most effective ways to combat COVID-19
Apart from the PCR test, there is an express diagnostics technology developed by Japanese Mirai Genomics and its Russian partner, Genetic Technologies. It includes both tests as such and portable diagnostic systems that can show results in no more than 30 minutes. A standard PCR test requires about 3–4 hours plus the time to transport the samples to the lab, so it is more time-consuming. The Russian-Japanese tests are based on SmartAmp isothermal molecular diagnostics. Essentially, it has the same principle as PCR and involves increasing the number of the virus’s DNA fragments, but the new method does not require heating and cooling at different stages of the process, which increases the reaction rate. The express diagnostics is eight times faster than the PCR, and its portable laboratory can test up to 20 patients per hour. Since testing is recognised as one of the most effective ways to combat COVID-19, developing and scaling up the relevant technologies will remain a priority in the near future.

According to WHO, the main coronavirus testing method is Polymerase Chain Reaction (PCR) testing (polymerase is an enzyme), which can detect the virus during the incubation period.
Polymeric infection barrier
The choice of protective means depends on the type of the microorganism. COVID-19 belongs to pathogenicity group 2, which includes pathogens of highly contagious human epidemic diseases. There are four such groups. Different pathogenicity groups, working conditions, and degrees of potential threat require different types and combinations of protective clothing.
The lens is made of 1 mm thick polycarbonate. Polycarbonate is a transparent polymer plastic
Anti-epidemic SMMS surgeon cap
Safety glasses
The lens is made of 1 mm thick polycarbonate. Polycarbonate is a transparent polymer plastic.
Respirator
The body is made of soft plastic, rubber or filter material, such as foam rubber (flexible polyurethane foam).
Medical mask
Spunbond, SMS
Protective trousers, jackets, overalls
SMMS
Disposable gloves
Gloves can be made from a variety of polymers, including latex, nitrile and vinyl.
Sleeves covers
SMMS
High boot covers
SMMS
Bag for contaminated clothing
Rubber fabrics. Durable material with textile foundation and vulcanised rubber coating.
Russia’s President Vladimir Putin visiting a hospital in Moscow. Different pathogenicity groups, working conditions, and degrees of potential threat require different types and combinations of protective clothing.
Materials
Spunbond is a non-woven material and the technology of its production from melted polymer. The raw material used is fiber forming polymers with a wide molecular weight distribution, such as polypropylene, polyethylene terephthalate (PET), polyamide and others.
Meltblown is a filter material (fine-grained nets of polypropylene fibres) that is comfortable to touch and gives strength and barrier properties.
SMS is a multi-layer nonwoven material with outer layers of spunbond and inner layer of meltblown.
SMMS is a four-layer nonwoven material of various densities, consisting of two layers of spunbond and two layers of meltblown.
So far, the transfusion of cured patients’ blood plasma has been the only specific treatment for COVID-19 patients
Searching for cure
Early detection and prediction using the test, as well as the search for a vaccine are definitely key to overcoming the pandemic, but thousands of infected people need medical help now. Chinese doctors, whose positive example is studied throughout the planet, officially recommended fighting the virus with Arbidol despite its ambiguous reputation. This antiviral drug suppresses influenza A and B viruses and has long proclaimed effectiveness against other viruses, such as coronovirus, in its description. Other recommendations include:
• chloroquine (antimalarial drug);
• ribavirin (an antiviral drug used for chronic hepatitis C and hemorrhagic fever);
• interferons (the common name for a number of proteins secreted by body cells in response to a virus);
• lopinavir + ritonavir (a combined antiviral therapy, mainly used against HIV).
Chinese doctors, whose positive example is studied throughout the planet, officially recommended fighting the virus with Arbidol despite its ambiguous reputation.
Scientists and doctors advise against using immunomodulators without prescription as irresponsible self-medication has nothing to do with professional experiments in hospitals
During the search and testing, close attention is paid to drugs that helped curb previous coronavirus outbreaks. Scientists are investigating drugs for infectious diseases with a similar mechanism of infection hoping to develop anticoronavirus therapy as soon as possible. So far, the transfusion of cured patients’ blood plasma has been the only specific treatment for COVID-19 patients. Antibodies formed in the human body help defeat the new virus.
Currently, there is not uniform treatment protocol or specialised drug, so doctors have to treat consequences, i.e. symptoms. Drugs that can enhance immunity are also used. In Russia, unlike Western countries, such medications are available over the counter and quite popular. However, scientists and doctors advise against using immunomodulators without prescription as irresponsible self-medication has nothing to do with professional experiments in hospitals. The effectiveness of immunomodulators in combating the new infection has not been confirmed. For instance, a poll conducted by Doctor At Work online platform showed that the majority of respondents find the existing evidence insufficient.
There is still an ongoing debate on immunomodulators in the Russian medical community and among Russians working abroad. No single approach has been extensively adopted. We conducted our own poll regarding the potential of the existing antiviral drugs to prevent COVID-19, and found out why medications stimulating immunity are so controversial.
Battlefield: immunomodulators
“These is no medicine that can prevent a disease caused by the coronavirus infection. There are no ways to prevent or treat COVID-19. Therefore, there is not much point in buying antiviral medications. Immunomodulators – even Oxolinum ointment – have no positive effect and are a waste of money. A person who used them might consider himself well-protected and act carelessly, which might result in his getting infected.
Meanwhile, the preventive measures are well known: do not leave home unless necessary, wash hands, face and nose thoroughly when you return; sanitise every item you bring in.
Pharmaceutical business is aimed, among other things, at profit making, so it sells immunomodulators if there is a demand for them. Drugs cannot boost immunity, but they can weaken it. Experimenting with immunity is usually fruitless and even dangerous in some cases.”
Thanks to modern technologies and digital solutions, as well as cross-functional scientific cooperation, we will soon develop state-of-the-art drugs and antiviral treatment methods.
“Russia saw a surge in demand for antiviral medication and immunomodulators as the epidemic broke out, while sales of certain drugs went up 3–5 times. The medical community takes a dim view of popular Russian immunomodulators and antivirals. I disagree with it.
Medications are effective to the extent they are properly applied. No drug is a cure-all, the problem lies in self-treatment when one attempts to medicate oneself without a diagnosis or medical expertise.
For now, there are no drugs that prove effective against the coronavirus, but studies of existing antivirals and certain antiparasitics show that some of them might demonstrate positive dynamics in treating COVID-19. Yet, again, they can only be applied upon prescription and under a doctor’s supervision.”
“Theoretically speaking, antiviral medications can be effective against the coronavirus. However, not enough research has been done on such treatment and its consequences. There is a lot of fuss about it now, but the most interesting findings are yet to come.
The key questions are whether the coronavirus can cause clinically silent infections and for how long patients remain immune after recovery. Take the influenza virus that we are already used to: it breaks out twice a year in late autumn and early spring and is asymptomatic in summer. I expect the coronavirus to result in a similar situation, as it is closely related to the flu.
Everyone is a carrier of multiple viruses and even the strongest immune system cannot ward off all the threats. Using immunomodulators is justified, given the absence of effective medications against coronavirus. But I believe that the best way to boost immunity is to maintain a well-balanced nutrition.”
“In case of coronavirus, the only cure is broad-spectrum antivirals. Although many medications have an immunomodulating effect, the major flaw of pharmaceutical drugs is that they are mostly designed for targeted application. Meanwhile, interferons, natural proteins, are an essential part of the innate immune system that helps protect the body against all kinds of viruses.
We developed and tested drugs that stimulate interferon induction in patients. I took part in creating Cycloferon, Kagocel and Viferon. Interferon inductors are mainly used to treat flu, Hepatitis B and C and herpes infections. However, the range of viruses they can actually suppress is much wider.
There are reasons to believe that they might also be effective in coronavirus prevention. Domestically produced drugs help fight influenza, and I think that interferon inductors are among the factors that prevent outbreaks of flu epidemics in Russia. Yet, the pharmaceutical market is a huge system wh ere every new medication is viewed sceptically with Russian developments often lacking trust.
Finally, it is self-evident that our immune system, the greatest natural gift, has its flaws. Add to that the need to boost the weakened herd immunity worldwide. Immunomodulators can help us improve our immune systems with the use of natural components.”
“Apparently, immunomodulators provide a certain effect which is often very powerful, but highly unpredictable, as no full-scale clinical trials have been ever conducted. Many medications lack accurate data. All prescriptions rely on a doctor’s opinion and expertise, yet no one has acquired enough experience to treat the novel coronavirus infection.
The doctor’s guess is obviously better than self-treatment, but the result is still unforeseeable. What is more, due to genetic variation each immune system has unique features and therefore in each case a personalised approach is needed to sel ect a proper medication. It is pointless and even harmful to use immunomodulators to prevent diseases.
An immune system can only be activated for a limited period of time, so why disturb it if you are unlikely to get sick? The use of such drugs is justifiable in two cases: you can feel the first symptoms of a disease, or you know for sure that you have had contact with an infected person.”
Bits of big science
The coronavirus has caused problems for both healthcare and economy sectors, so current forecasts are diverse. One thing is clear: viruses will co-exist with us and mutate from time to time, forcing us into an ongoing fight against them.
Experts are confident that beating COVID-19 is just a matter of time
It is well-known that chemistry discoveries used by healers of the past became the foundation of modern medicine. Organic synthesis built the basis for the pharmaceutical industry. Apart fr om organic compounds (herbs, oil, natural gas), medical production also uses inorganic components (ores, gases, water). The evolution of synthetic organic chemistry unlocked opportunities for creating new pharmaceuticals to treat diseases that had been considered incurable before. This illustrates how chemistry and medicine stick together to reach common goals.
The constant growth in the number of individual chemical compounds studied by scientists helps synthesise new medications. While remaining focused on a number of diseases, pharmacists had to prioritise viral infections due to the pandemic. Experts are confident that beating COVID-19 is just a matter of time. Thanks to modern technologies and digital solutions, as well as cross-functional scientific cooperation, we will soon develop state-of-the-art drugs and antiviral treatment methods.
Source: the All Chemistry magazine
Download PDF















Vasily Vlassov
MD, Vice-President of the Society for Evidence Based Medicine